Latest from the blog
How to get the most out of your preventive screenings at no extra cost to you
Taking care of your health is important. One way to stay healthy is by getting regular checkups and screenings. Many preventive screenings are covered at no cost when you have health insurance through Access Health CT (AHCT). Here’s how to make the most of these...
Moving to Connecticut? Here’s How to Enroll in Health and Dental Coverage through Access Health CT
If you’re moving to Connecticut and you don’t have health or dental coverage, or if you’re unsatisfied with your current coverage, you may qualify for health and dental coverage through Access Health CT (AHCT). AHCT is the state’s official health insurance...
How to Report Life Changes to Access Health CT and Why It’s Important
Life can change in many ways. You might have a change in income (how much money your household makes), get married or have a baby. When these things happen, it’s important to tell Access Health CT (AHCT) right away. Reporting life changes will help you get the right...
Navigating health coverage when you’re self-employed: A guide to Access Health CT options
Being self-employed means you can set your own schedule and be your own boss. But it also means that you may need to find your own health or dental coverage. Access Health CT (AHCT) is here to help you get the coverage you need.Understanding coverage If you’re...
How and why you need to verify your personal information with Access Health CT
When you apply for health coverage through Access Health CT (AHCT), we might ask you to provide certain documents to verify your personal information. These are called verification documents. They help us check important information like your household income,...
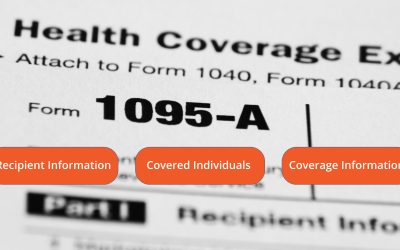
Look for Form 1095-A from Access Health CT to file your Federal Income Tax Return
Tax season is here. If you were enrolled in health insurance through Access Health CT (AHCT) last year, you’ll need Form 1095-A to file your federal income tax return. This Form has details about your health plan and any financial help you received. Keep it safe, just...